CARE
PLANS
PART 2: THE CURRENT LANDSCAPE
This piece is a continuation of the Care Plan series. While Part 1 focused on what care plans are and how they came about, this article will explore how care plans are currently being used in the health space.
The Process of a Care Plan
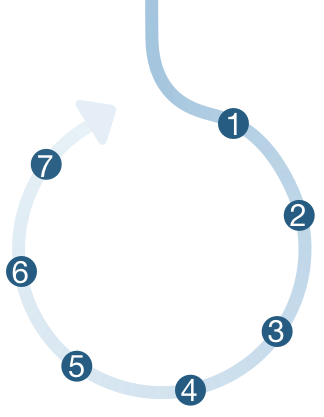
There is not yet any clinically recognized universal standard for care plan creation and implementation. But using elements derived from CMS’s Meaningful Use Stage 2 requirements,1,2 the Coordinated Care Plan documentation from the Ontario Medical Association,3 the traditional nursing care plan structure,4 and the Care Plan Glossary from the ONC’s Standards and Interoperability Framework,5 we have created a generalized care plan journey map below.
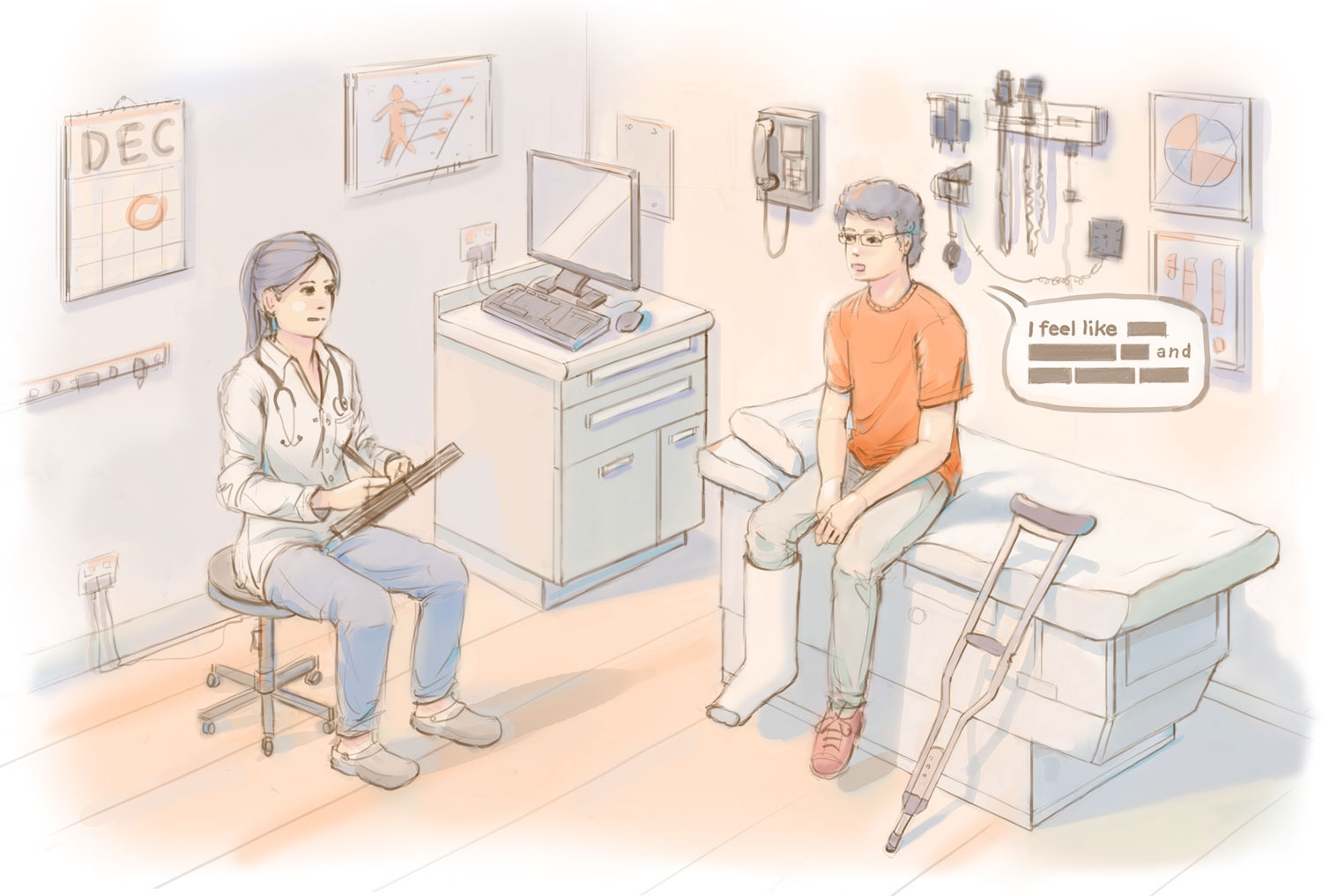
The journey begins with a patient visiting his primary care doctor.



Understand Health History
The beginning of any care plan process, whether creation or review, requires an understanding of the patient’s health history. This should be summative in nature, and include basic information such as demographics, care team, vitals, problems, allergies, medications, therapies, notable encounters or procedures, and an indication of whether an advance care plan is in place. It is important to keep a patient summary up to date so that any care professional can reference it in an emergency.
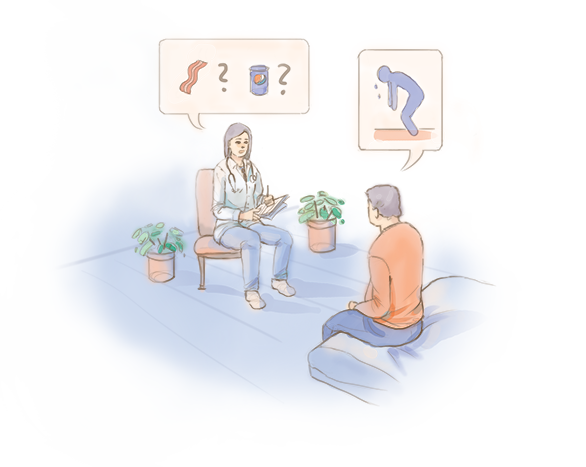
Identify Health Concerns
The next step is to identify what the current problems or health concerns are. This can involve reviewing symptomology, eating habits, physical activity, sleep habits, psychological issues, management of medication, sexual health, cessation of bad habits, management of any other daily activity, or any social or environmental factors on health. Collection of vitals might also be involved in the identification of health concerns.
Set Goals
Goals are set to improve or resolve the identified health problems by the next review period. SMART goals (specific, measurable, achievable, realistic, time oriented) help break down goals into smaller specific steps. Goals should also be measured in a way that’s quantifiable so that changes can be seen over a pratice timeframe. These can include both patient defined goals such as longevity, function, comfort, etc., and clinician defined goals.
Instruct and Intervene
After the desired outcomes are specified, the interventions and instructions on how to acheive those goals can be delivered. Instructions are educational directions to the patient/other providers about how to care for the patient's condition, what to do at home, when to call for help, additional appointments, testing, medication changes/instructions, among others. Interventions are specified actions taken as steps toward achieving care plan goals. This can include adminstration of physical treatment, creation or adjustment to the medication plan, prescribed activities or community/social services, or removal of barriers to success.
Enlist Care Team
A team of individuals should be enlisted in the care of the patient. The care team includes both professional parties who manage and/or provide care, including medical practitioners, nurses, allied health practitioners (physiotherapist, speech therapist psychologist, pharmacist, etc.), social workers, and care managers; as well as non-professional members such as caregivers, family, friends, and the patient themselves. It should be determined by the patient which care team members are granted access to his or her health information.
Specify Outcomes to Review
It is important to set a specfic time for review of the care plan to determine whether patient needs are being met and if adjustments need to be made. Low level, relatively healthy individuals may only need an annual review of the care plan, whereas those with more severe chronic illnesses may need a much more frequent checkup. Specific metrics for followup should be determined based on the health concerns and goals set.
Live the Care Plan
The most important part of the care plan process is how the patient implements it. They must translate guidance from their brief interactions with clinicians into sustained lifestyle behaviors to improve their own health. Self care makes up over 99% of healthcare, and it is only successful with a good care plan.
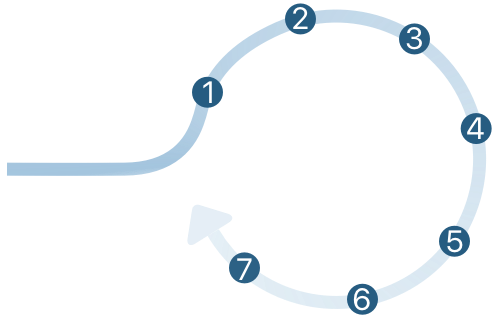
The process is a cycle. Patients live the care plan until the next medical encounter.
Understand Health History
The beginning of any care plan process, whether creation or review, requires an understanding of the patient’s health history. This should be summative in nature, and include basic information such as demographics, care team, vitals, problems, allergies, medications, therapies, notable encounters or procedures, and an indication of whether an advance care plan is in place. It is important to keep a patient summary up to date so that any care professional can reference it in an emergency.
Identify Health Concerns
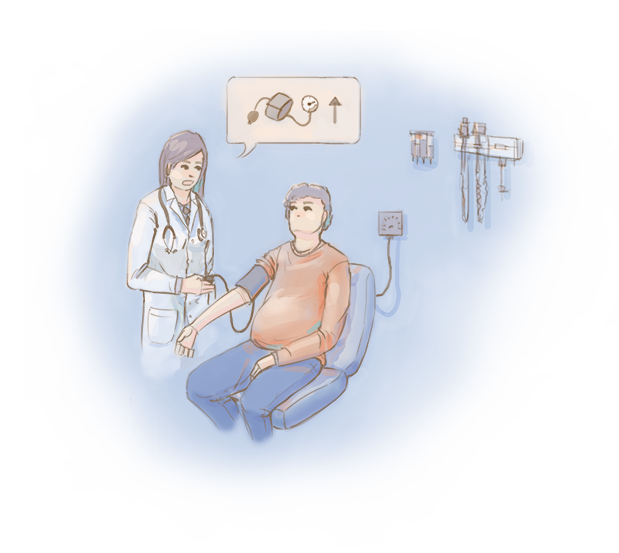
The next step is to identify what the current problems or health concerns are. This can involve reviewing symptomology, eating habits, physical activity, sleep habits, psychological issues, management of medication, sexual health, cessation of bad habits, management of any other daily activity, or any social or environmental factors on health. Collection of vitals might also be involved in the identification of health concerns.
Set Goals
Goals are set to improve or resolve the identified health problems by the next review period. SMART goals (specific, measurable, achievable, realistic, time oriented) help break down goals into smaller specific steps. Goals should also be measured in a way that’s quantifiable so that changes can be seen over a pratice timeframe. These can include both patient defined goals such as longevity, function, comfort, etc., and clinician defined goals.
Instruct and Intervene
After the desired outcomes are specified, the interventions and instructions on how to acheive those goals can be delivered. Instructions are educational directions to the patient/other providers about how to care for the patient's condition, what to do at home, when to call for help, additional appointments, testing, medication changes/instructions, among others. Interventions are specified actions taken as steps toward achieving care plan goals. This can include adminstration of physical treatment, creation or adjustment to the medication plan, prescribed activities or community/social services, or removal of barriers to success.
Enlist Care Team

A team of individuals should be enlisted in the care of the patient. The care team includes both professional parties who manage and/or provide care, including medical practitioners, nurses, allied health practitioners (physiotherapist, speech therapist psychologist, pharmacist, etc.), social workers, and care managers; as well as non-professional members such as caregivers, family, friends, and the patient themselves. It should be determined by the patient which care team members are granted access to his or her health information.
Specify Outcomes to Review
It is important to set a specfic time for review of the care plan to determine whether patient needs are being met and if adjustments need to be made. Low level, relatively healthy individuals may only need an annual review of the care plan, whereas those with more severe chronic illnesses may need a much more frequent checkup. Specific metrics for followup should be determined based on the health concerns and goals set.
Live the Care Plan
The most important part of the care plan process is how the patient implements it. They must translate guidance from their brief interactions with clinicians into sustained lifestyle behaviors to improve their own health. Self care makes up over 99% of healthcare, and it is only successful with a good care plan.
The process is a cycle. Patients live the care plan until the next medical encounter.
The Care Plan Product Landscape
As of January 2015, CMS transitioned Medicare to the more quality-based practice of reinbursing for care management of eligible patients with 2 or more chronic conditions. Now, physicians, certified nurse specialists, nurse practitioners, and physician assistants are incentivized to perform 20 minutes of non-face-to-face care coordination services for every Medicare-qualifying patient each month. This can include tasks such as recording and coordinating patient health information (even from outside their own practice), managing care transitions (such as discharge from a hospitalization), coordinating clinical home or community services, systematic assessments of patient needs, and finally, the creation and review of a perpetually accessible comprehensive care plan. Now that Medicare has begun this transition, other private insurance companies are beginning to follow suit to prioritize consistent, preventative care facilitated by patient-accessible care plans. As a result, many care planning services have emerged to address the software needs of care management.
This matrix aims to explore the effectiveness of current care plan services based on defined criteria. Each service was scored based on the percentage of criteria met in each of the eleven topic areas. A 0 means that none of the criteria points were fulfilled. Click on each criteria at the top of the matrix to break down what subcriteria were used for scoring. The final score, out of 100, is the average of the service’s scores in each criteria area.

|
50Interoperability | 50Patient Summary | 80Education | 60Goal Setting | 25Vitals Tracking | 50Dynamic Intervention | 75Data Ownership | 43Prof. Team Comm. | 0Non-prof. Team Comm. | 100Clinical Validity | 50Content Breadth | 53.00Average |

|
33 | 25 | 60 | 80 | 50 | 50 | 75 | 0 | 0 | 75 | 75 | 47.55 |

|
20 | 25 | 60 | 80 | 0 | 0 | 75 | 86 | 17 | 50 | 100 | 46.64 |

|
40 | 75 | 20 | 0 | 25 | 0 | 75 | 71 | 0 | 75 | 100 | 43.73 |

|
20 | 50 | 0 | 40 | 0 | 0 | 50 | 14 | 66 | 0 | 30 | 24.55 |
|
80 | 100 | 20 | 40 | 50 | 0 | 100 | 29 | 83 | 25 | 100 | 57.00 |

|
80 | 50 | 20 | 80 | 0 | 0 | 75 | 0 | 100 | 25 | 30 | 34.55 |

|
100 | 75 | 40 | 20 | 0 | 0 | 75 | 57 | 0 | 50 | 70 | 44.27 |

|
40 | 100 | 25 | 20 | 0 | 0 | 75 | 29 | 0 | 0 | 70 | 32.64 |

|
80 | 75 | 40 | 0 | 25 | 0 | 50 | 43 | 0 | 0 | 70 | 34.82 |

|
80 | 50 | 0 | 0 | 25 | 0 | 75 | 29 | 0 | 50 | 80 | 35.36 |

|
80 | 50 | 20 | 60 | 100 | 0 | 100 | 29 | 0 | 50 | 100 | 53.55 |

|
0 | 25 | 40 | 0 | 25 | 50 | 75 | 29 | 0 | 0 | 80 | 29.45 |

|
83 | 75 | 20 | 20 | 25 | 0 | 100 | 29 | 0 | 50 | 70 | 42.91 |

|
60 | 50 | 0 | 0 | 50 | 0 | 75 | 29 | 0 | 0 | 70 | 30.36 |

|
83 | 0 | 60 | 60 | 25 | 0 | 50 | 0 | 0 | 25 | 10 | 20.91 |

|
33 | 25 | 0 | 0 | 75 | 0 | 50 | 0 | 0 | 0 | 100 | 25.73 |
There is a clear distinction between patient portal services (Bridge, Patient Fusion, Intelichart) focused on data interoperability, health history, and professional care team communication; and the less clinical services (CareZone, Healthtap, Wellframe, Healarium) focused on patient engagement, goal setting, and non-professional care team communication. Wellframe, CareSync, and HealthVault are the few services that attempt to bridge the gap between those two focuses, putting them at the top of ranking as the more successful care plan services.
However, certain deficits seem to be shared by almost all of these services. While interoperability is a growing focus, there still seems to be trouble in adopting a universal data standard for content and holding services to consistent clinical quality metrics. Many services successfully incorporate data tracking and visualizations, though there is virtually no presence of actual insight from this data. Users are not receiving projected outcomes or recommendatons for behavior change based on collected data. Similarly, while users can access all of their health data, they rarely get to ‘own’ it. This means being presented the raw data for export, sharing, and personal documentation.
These limitations, and others collected through secondary literature research are explored further below.
The Care Plan Product Landscape
This matrix aims to explore the effectiveness of current care plan services based on defined criteria. Each service was scored based on the percentage of criteria met in each of the eleven topic areas. A 0 means that none of the criteria points were fulfilled. Click on each criteria at the top of the matrix to break down what subcriteria were used for scoring. The final score, out of 100, is the average of the service’s scores in each criteria area.
The Barriers to Care Planning
The Next Steps for Care Plans
Care plans have come a long way since their conception. We have created a somewhat systematic approach to a patient health guide, yet have not standardized it for consistant communication and delivery of care. We have established appropriate intervention steps for a variety of diagnosed conditions, yet have not mastered the format and delivery of these steps so that they are effective and engaging to patients. We have figured out how to collect massive amounts of crucial patient health data, yet we have not offered that data to the patient to carry with them and seamlessly share throughout their diverse medical encounters. We are only on the cusp of the health technology wave, and care plans have a bright future ahead of them. Want a glimpse? Check out our next feature.
Authors
Contributors

Web Designer & Developer
Yanyang Zhou

Web Designer & Developer
Jennifer Patel
@catamariface

GoInvo, MIT
Juhan Sonin
@jsonin

University of Missouri | toomanyclicks.com
Jeff Belden, MD
@jeffbelden

University of Michigan
Joyce Lee, MD, MPH
@joyclee

THINK-Health | Health Populi blog | Huffington Post
Jane Sarasohn-Kahn, MA, MHSA
@healthythinker

Healthcare Provocateur
Harry Sleeper
@harrysleeper
References
- 1. “Stage 2 Meaningful Use Core Measures”. (2015, August). Retrieved from https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/Stage2_EPCore_15_SummaryCare.pdf
- 2. United States, Department of Health and Human Services. “Chronic Care Management Services”. S(2015, May). Centers for Medicare and Medicaid Services. Retrieved from https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/ChronicCareManagement.pdf
- 3. “Key Elements to Include in a Coordinated Care Plan”. OMA. (2014, June). Retrieved November/December, 2015, from https://www.oma.org/Resources/Documents/CoordinatedCarePlan_June2014.pdf
- 4. “NHS Guide to long-term conditions and self care: What is a care plan?” (n.d.). Retrieved December 21, 2015, from http://www.nhs.uk/Planners/Yourhealth/Pages/Careplan.aspx
- 5. General Information. (n.d.). Retrieved December 25, 2015, from http://wiki.siframework.org/LCC Longitudinal Care Plan (LCP) SWG
- 6. Circle of Care. (2015, August). Retrieved December 25, 2015, from https://www.ipc.on.ca/images/Resources/circle-of-care.pdf
- 7. Palmieri, J. J., & Stern, T. A. (2009). Lies in the Doctor-Patient Relationship. Prim. Care Companion J. Clin. Psychiatry The Primary Care Companion to The Journal of Clinical Psychiatry,11(4), 163-168
- 8. Better communication between caregivers reduces medical errors, study finds. (n.d.). Retrieved December 20, 2015, from https://med.stanford.edu/news/all-news/2014/12/better-communication-between-caregivers-reduces-medical-errors.html
- 9. Resource Careplan. (n.d.). Retrieved December 20, 2015, from https://www.hl7.org/fhir/careplan.html
- 10. How to Deal with Conflicting Advice from Healthcare Professionals. (n.d.). Retrieved January 25, 2016, from http://www.brainline.org/content/2009/06/how-to-deal-with-conflicting-advice-from-healthcare-professionals.html
- 11. Garson, A., Green, D. M., Rodriguez, L., Beech, R., & Nye, C. (2012). A New Corps Of Trained Grand-Aides Has The Potential To Extend Reach Of Primary Care Workforce And Save Money. Health Affairs, 31(5), 1016-1021.
- 12. Wellframe. (n.d.). Retrieved December 19, 2015, from http://www.wellframe.com/
- 13. Healarium. (n.d.). Retrieved December 15, 2015, from http://www.healarium.com/
- 14. HealthTap. (n.d.). Retrieved December 17, 2015, from https://www.healthtap.com/
- 15. Amwell. (n.d.). Retrieved December 21, 2015, from https://amwell.com/
- 16. CareZone | Easily organize health information in one place. (n.d.). Retrieved December 22, 2015, from https://carezone.com/home
- 17. Caresync. (n.d.). Retrieved December 20, 2015, from http://www.caresync.com/
- 18. Caring in Place. (n.d.). Retrieved December 20, 2015, from http://caringinplace.com/website/index.html
- 19. Patient Portal Software for Hospitals and Physicians :: Bridge Patient Portal. (n.d.). Retrieved December 19, 2015, from http://www.bridgepatientportal.com/
- 20. Inxite Health Systems. (n.d.). Retrieved December 20, 2015, from https://www.inxitehealth.com/
- 21. My Care Plan. (n.d.). Retrieved December 17, 2015, from http://www.journeyforward.org/planning-tools/my-care-plan
- 22. Online Patient Portal Software - InteliChart. (n.d.). Retrieved December 22, 2015, from http://www.intelichart.com/
- 23. Microsoft HealthVault. (n.d.). Retrieved December 20, 2015, from https://www.healthvault.com/us/en
- 24. Patient Fusion. (n.d.). Retrieved December 18, 2015, from https://www.patientfusion.com/
- 25. Epic: Mobile Applications and Portals. (n.d.). Retrieved December 20, 2015, from https://www.epic.com/software-phr.php
- 26. AskMD. (n.d.). Retrieved December 28, 2015, from https://www.sharecare.com/askmd/get-started
- 27. Medfusion Plus - Medfusion. (n.d.). Retrieved December 21, 2015, from http://www.medfusion.com/solutions/medfusion-plus/