CARE
PLANS
PART 3: The Future
Digital is Better
Distance and remote based care is growing with the continuing expansion of smartphone device consumption and installation of broadband services into homes and businesses.1,2 Expansion of free internet services, such as in the UK, where the National Health Service (NHS) will be converted into a free wi-fi zone, are also a driver of this digitization trend.3 With better connectivity, internet speeds, and smart monitoring devices, there may soon be a shift from the traditionally episodic, face-to-face care to a model where the immediate, remote, and individualized care plan is possible.4 Patients will be able to more consistently access, collaborate on, and adjust their care plans at home, work, school, while traveling, and in mobile clinics.5 This shift is especially important for less mobile and more vulnerable demographics such as new borns, physically disabled people, or seniors.6,7
Standardized, Interoperable Content
MITRE Engine →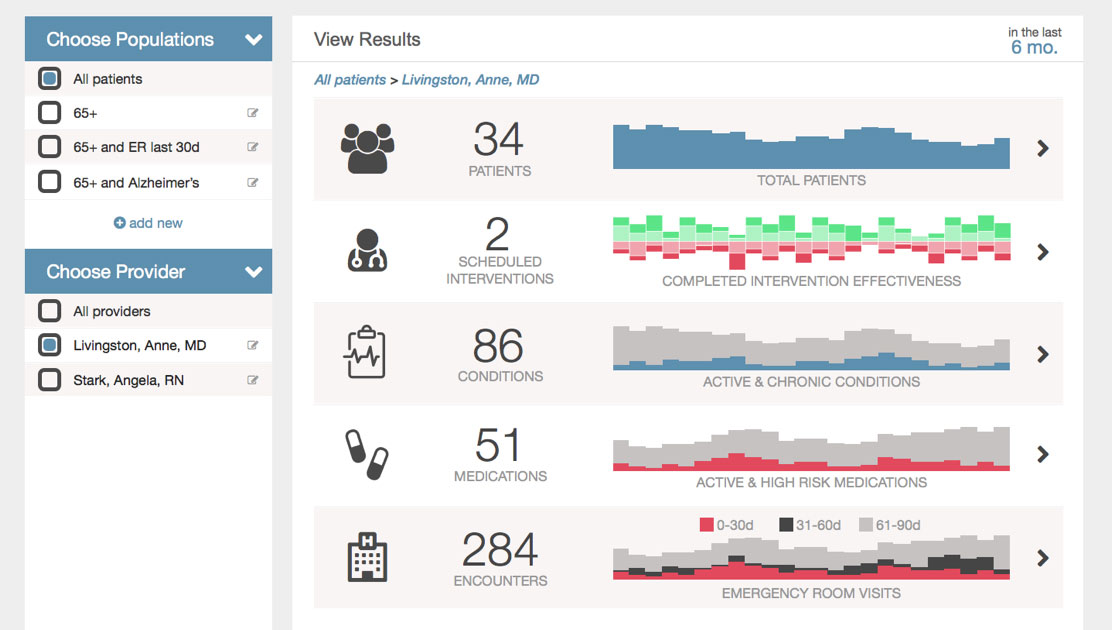
There must be more consensus on care plan content. All this variation leads to miscommunication and errors in the transfer of care.
Standardization of care plans throughout the spectrum of health concerns will aid in communication and collaboration across care team members over time, providing high-quality longitudinal care with reduced risk for medical error.2,8,9 If medical community leaders converge to develop clinical pathways into a library of robust care plan templates, they can then be customized to each patient’s needs while still being interoperable among all care organizations.10,11,12 Using consistent quality metrics, the effectiveness of these templates can be assessed to identify how they must evolve and improve.
Photo by Philips Communications
"Give Me My Data"
There needs to be an EMR system that can aggregate medical records, lab tests and scans, genomic data, and all other health data (including patient-generated) and analyze them in a meaningful way.
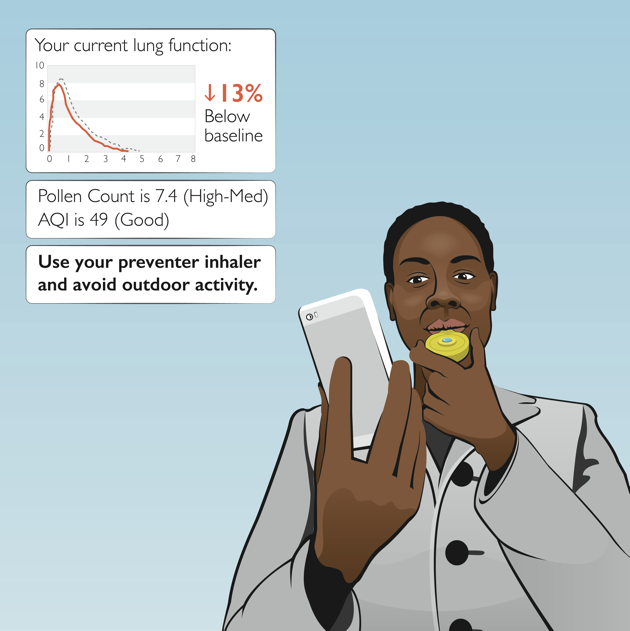
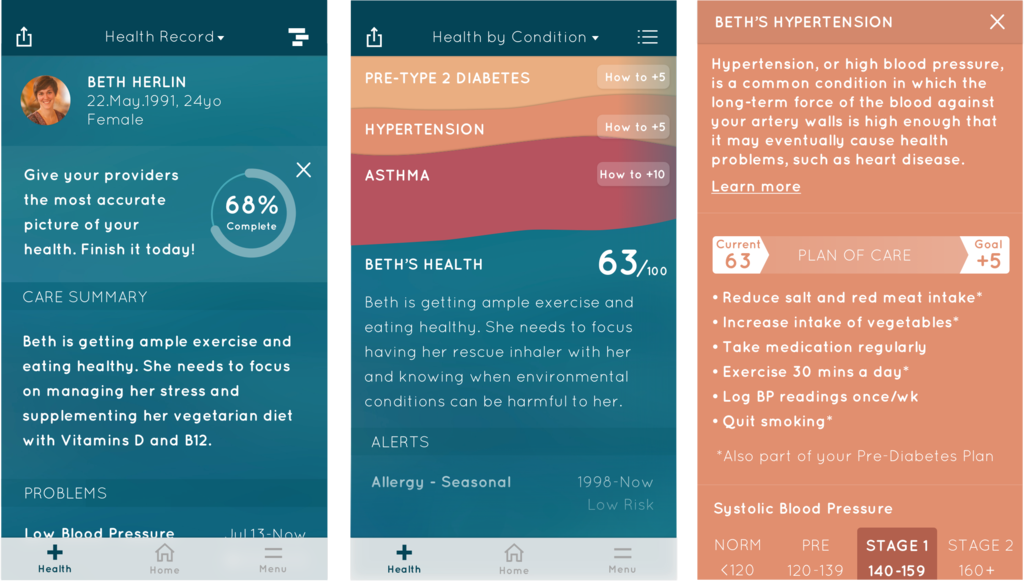
Patients will have an unlimited and ever-evolving reservoir of data collected from embedded devices, mobile phones, and other sensors that is then synthesized into an understandable personal health score.13 Predictive analytics will help identify patterns in this data to create actionable insights and recommendations for care plan adjustments. With the advent of human genome mapping, we can further fine tune care plans according to patient's family medical history and genetic predispositions. In a broader context, we can look at the population's genetic data comparatively to differentially diagnose various health conditions.14 Once we can move past the stigma of sharing health record information with patients and the complexity of securing the information from harm, we can approach the ideal world where patients are the rightful owner of their health data, using it maintain a holistic view of their health.6,13,15
There needs to be an EMR system that can aggregate medical records, lab tests and scans, genomic data, and all other health data (including patient-generated) and analyze them in a meaningful way.
Empowered Patients are
Activated Patients
We need care plans to be more than list of instructions. They need to serve as a continuous source of diagnosis, relevant education, informative insights, and encouragement to take action.
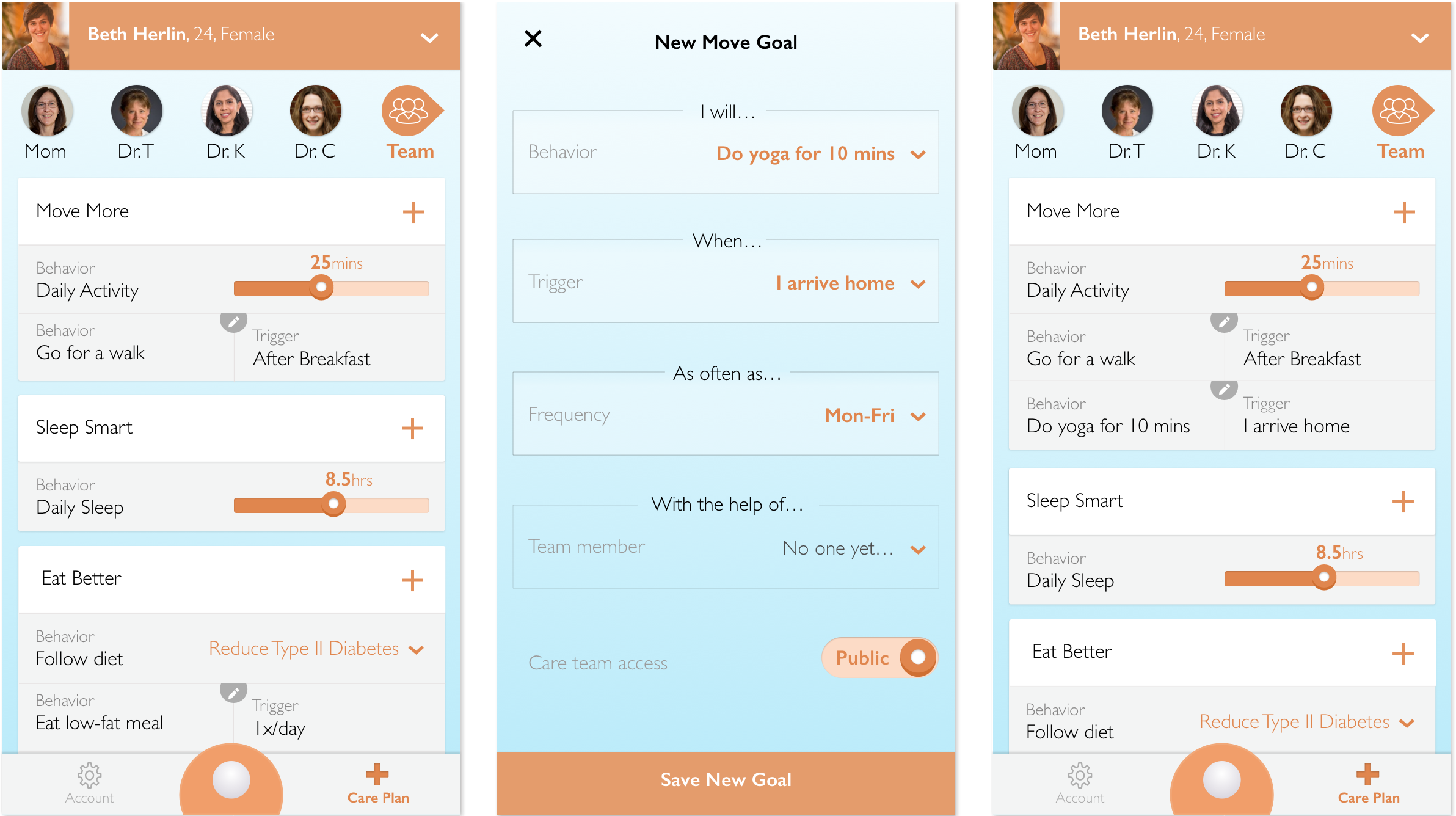
Patients should never leave a doctor’s office empty handed. Building an accessible digital care plan together with their provider will allow for both a more active discussion and a more empowered patient. When the patient feels a part of the decision making process and concludes a medical encounter feeling valued, knowledgeable, and supported by an accessible digital care plan, their likelihood of compliance to healthier 'self care' behaviors will grow.13 Similar engagement of caregivers will grow compliance even further as these more consistently present care team members are informed and empowered to help implement the care plan.10
Expanding the Meaning of Care Team
A more holistic approach to care planning suggests a greater need for cohesive inclusion of the patient's direct network into their care team.
In order to achieve better engagement and adherence to care plans, non-professional caregivers (friends and family) will be incorporated into the care team.16,17 These team members have the highest degree of access to the patient, and the most incentive to provide care. Services that expand education and engagement to both the patient AND these members will emerge to fully utilize this component of the care team.18
Another important presence in this expanding care team is the online community. We will start to see services that incorporate community forums and population analytics to take advantage of the the wealth of knowledge and experience of similar patients.18
The advancement of digital care plans has surfaced the need for new healthcare roles that bridge the gap between providers and patient-facing technology. One emerging role, the nurse extender clinical aide, or grand-aide, interacts more frequently with patients to ensure adherence to the care plan and keeps the more highly-trained providers informed about the status of the patient.19
Dynamic Plans Evolve
With the Patient
Full Poster
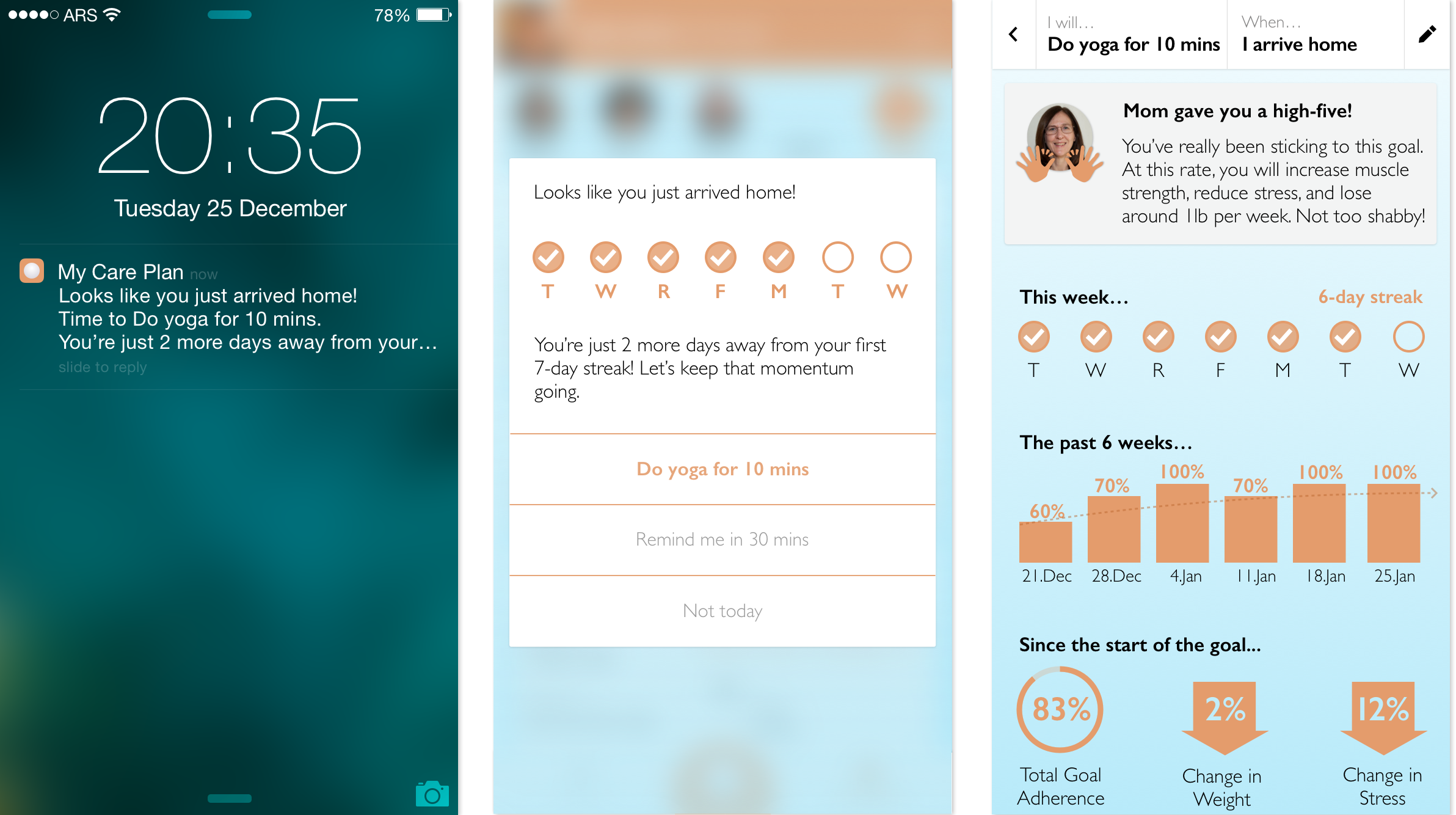
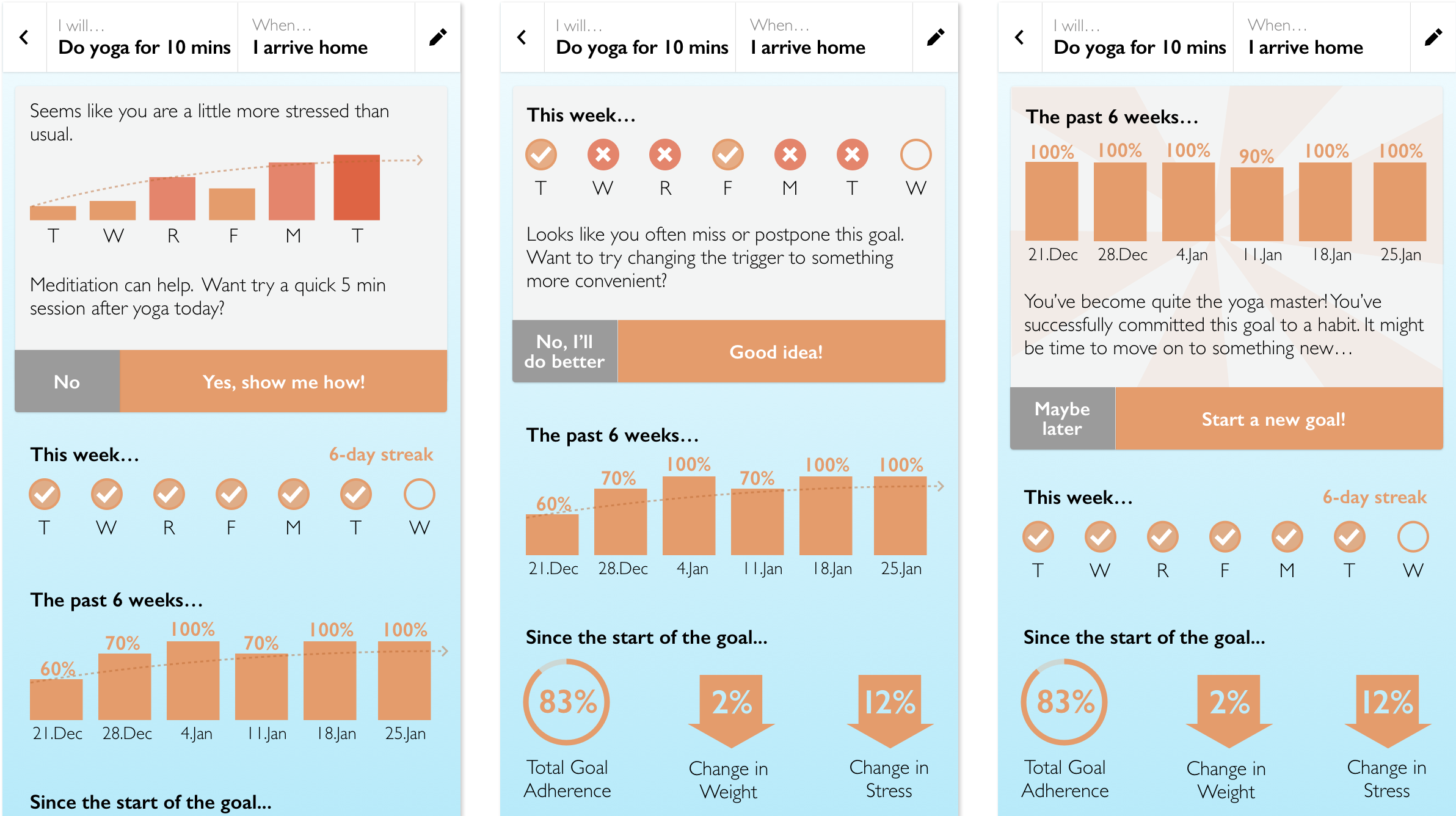
Patients need more diagnosis, goal setting, and guidance than an annual check up with their doctor in order to engage in effective, preventative self care.
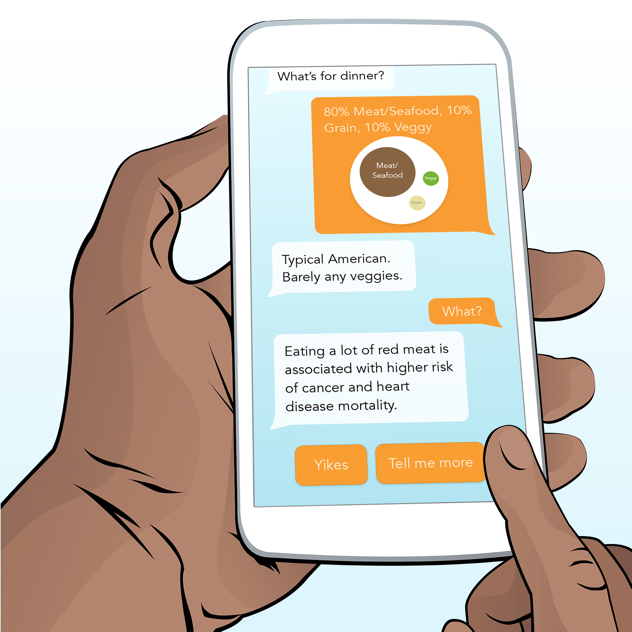
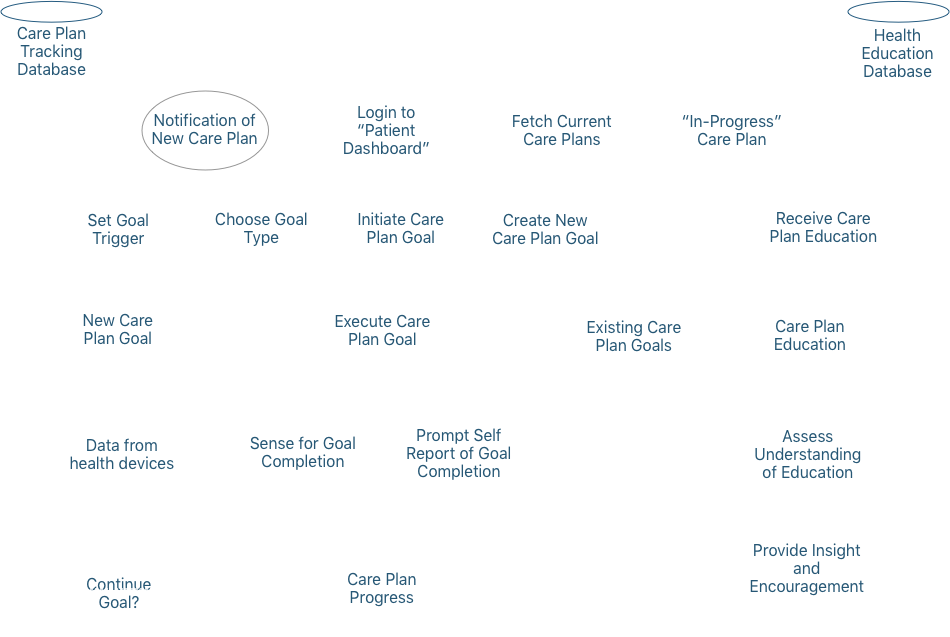
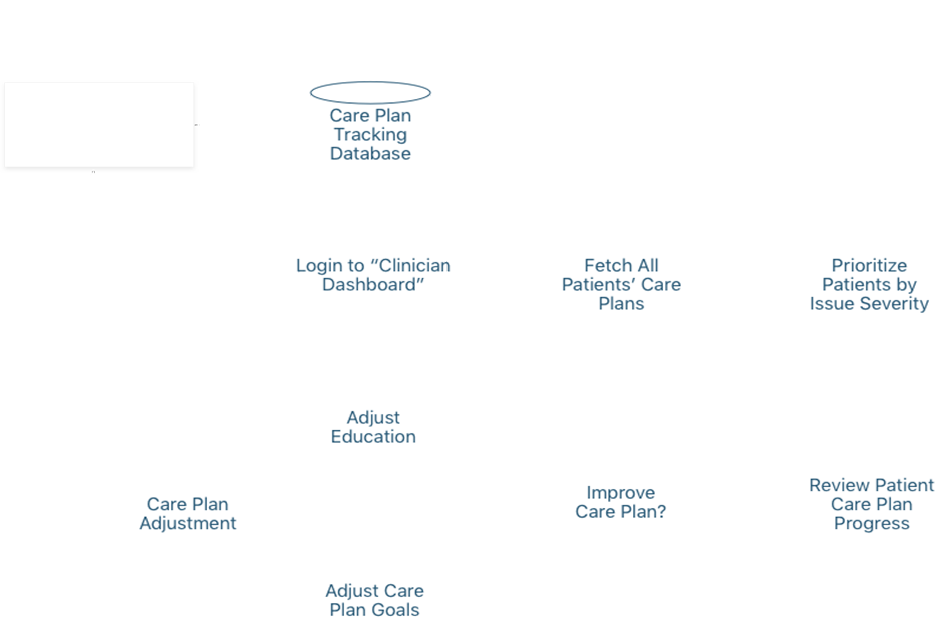
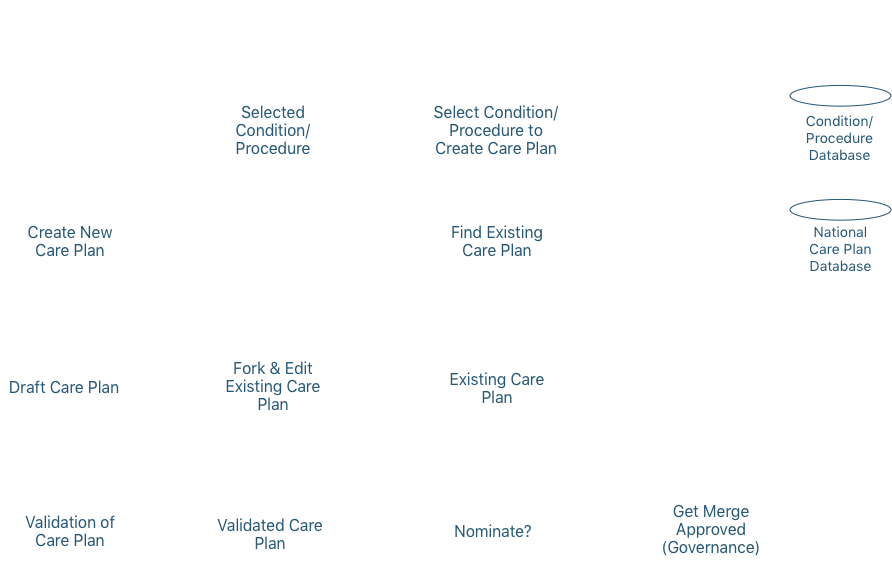
As digital care plans gain the ability to deliver personalized health content (including goals) and collect relevant metrics, the opportunity arises to coalesce these functions into a feedback loop.15 This means the care plan will facilitate a prescribed or selected care plan with specified goals, assess relevant data from vitals sensors, the environment, or behaviors, to determine if the goal criteria is met, and then auto-adjust the care plan goals and education accordingly. Health scores and predictive analytics will be used to aid engagement and understanding of the care plan and any changes to it. The use of patient health projections and relevant recommendations creates a kind of intervention engine that could behave autonomously from medical providers, though it could always be augmented and further personalized when clinician input is available. However, the concept of an intervention engine is dependant on a clinically-validated database of interoperable care plans.
Health Care is Shifting
The expansion of health coverage and the growing influx of patients will force a significant shift in the way healthcare is provided.21,22 More patients means a need for more providers. This will expand the roles and responsibilities of nurses, physician’s assistants, and other lesser-trained professionals, to provide more continuous care to more patients at one time.21 It also illuminates the benefit of utilizing the non-professional side of the care team, such as family caregivers and the online community in the care plan.
Healthcare payers are transitioning from a volume-based to value-based payment model, meaning that medical professionals will only get paid for the success of care, rather than for conducting the care itself.23 This shift requires quality metrics to assess outcomes, which can only be achieved through consistently delivered care plans and comprehensive health data tracking. When the feedback loop of an intervention engine is achieved, effectiveness of standardized interventions can be understood to accurately provide reimbursement and improve national healthcare as a whole.
Digital, standardized, dynamic, care plans will both augment effectiveness of our limited supply of medical professionals, and empower patients to engage in cost-effective, preventive self care behaviors.24
So… How Do We Get There?
It is unreasonable to expect to implement all of these care plan elements at once. Cost, both in conducting and implementing the future of care plans, also require further consideration. Below is a strategic view of what needs to be done.
Culture Shift
- Patients are the most important part of their care team, include them in the care planning process.
- Transparency in all medical encounters, give patients their data.
- The non-clinical part of the care team such as health coaches, family caregivers, and other networks are just as important. Rope them into the process more.
National Standards
- Synthesize research in the medical community and nationally establish a library of condition-specific care plans which can be consistently implemented in a patient-clinician encounter, and independently by the patient and other care team members.
Technology & Accessibility
- Make digital health sensors and devices that help track complex chronic conditions more affordable.
- Grow engaging health software solutions that improve accessibility and quality of care and actually get people to change behavior.
- Utilize payers’ risk scoring to create clinically valid patient-facing health score.
Create an Intervention Engine
In conjuction with the development of these technological advancements and national standards, we can start to create an autonomous engine that collects data relevant to chronic conditions, synthesizes it into meaningful information, interfaces with the national care plan library to select appropriate adjustments and recommendations, and delivers these recommendations along with any manual clinician input in an engaging way to patient and their care team. This engine is not meant to replace interaction with clinicians, but rather, augment it by providing continuous care in between medical encounters. Crucial to such an engine is the ability to compare assessed outcomes with interventions made to understand effictiveness across the entire population of patients. This will allow the engine to ‘learn’ and evolve, providing better and better care.
A Call to Action
To be successful on our journey towards digital care plans, we need your help.

Patients, Otherwise Known as “People”
- Take part in building your care plan with your doctor. You’re the most knowledgable part of your care team.
- Ask questions. Be informed.
- Take responsibility for your own health. Live your care plan.

Healthcare Designers & Entrepreneurs
- Adopt FHIR. It’s the lesser of all evils for now. Data MUST be interoperable.
- Know the clinical workflow. Your product should be a no-brainer for doctors, patients, and proxies.
- Give patients and their team authorship in the care plan process.

Medical Community
- Patient engagement is worth the investment. Activated patients behave in healthier ways.
- Transparent communication and complete accessbility to data make for more informed, healthier patients.
- Consider building a broader care team for the patient that leverages the expertise of health coaches, family, and community networks, and facilitates communication between clinic visits.
- Collect evidence and adjust care to get better outcomes. Value-based care is taking over Medicare payments (50% by 2018).

Policy Makers
- Single payer - We can’t better health until there is equal accessibility to care.
- Single standard - Meaningful Use 4 (or the next ONC health guidance as MU might be replaced) needs to dictate a national health data standard.
- National Care Plan Database - There should be clinical standards of care.
- Cost of Care Plans - Determine cost of ownership and creation of these future Care Plans, to contribute a standardized financial benchmark within a national care plan database.
Authors
Contributors
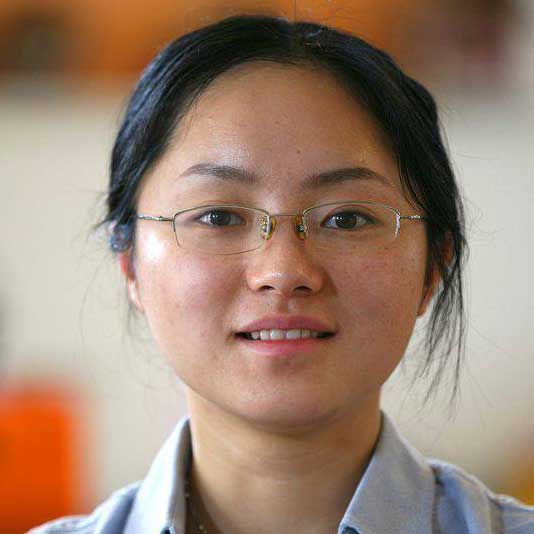
Web Designer & Developer
Yanyang Zhou

Web Designer & Developer
Jennifer Patel
@catamariface

GoInvo, MIT
Juhan Sonin
@jsonin

University of Missouri | toomanyclicks.com
Jeff Belden, MD
@jeffbelden

University of Michigan
Joyce Lee, MD, MPH
@joyclee

THINK-Health | Health Populi blog | Huffington Post
Jane Sarasohn-Kahn, MA, MHSA
@healthythinker

Healthcare Provocateur
Harry Sleeper
@harrysleeper
References
- 1. Device Ownership Over Time. (2013). Retrieved November 19, 2015, from http://www.pewinternet.org/data-trend/mobile/device-ownership/
- 2. U.S. Smartphone Use in 2015. (2015). Retrieved October 10, 2015, from http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/
- 3. Mental Health Network. (2014). [Brochure]. Author. Retrieved September 28, 2015, from http://www.nhsconfed.org/~/media/Confederation/Files/Publications/Documents/the-futures-digital.pdf
- 4. Aronson, L., Bautista, C. A., & Covinsky, K. (2015). Medicare and Care Coordination. Jama, 313(8), 797.
- 5. Lee, V. C. (2014). Mobile Devices and Apps for Health Care Professionals: Uses and Benefits.Pharmacy and Therapeutics, 39(4), 356-364.
- 6. NHS England » Putting digital to work for patients Tim Kelsey. (n.d.). Retrieved September 28, 2015, from https://www.england.nhs.uk/2015/06/tim-kelsey-10/
- 7. Center for Technology and Aging. (2009). Technologies for Remote Patient Monitoring in Older Adults [Brochure].
- 8. “LCC Longitudinal Care Plan (LCP) SWG”. S&I Framework. Retrieved from http://wiki.siframework.org/LCC+Longitudinal+Care+Plan+%28LCP%29+SWG?responseToken=09cf7263041efc0aaad547d5b2bd401fd
- 9. American Association of Nurse Life Care Planners. (2015). Scope and Standards of Practice[Brochure]. Author. Retrieved September 28, 2015, from http://nursingworld.org/DocumentVault/NursingPractice/Life-Care-Planning-Scope-and-Standards.pdf
- 10. Key Elements to Include in a Coordinated Care Plan [Brochure]. (2014). Retrieved from https://www.oma.org/Resources/Documents/CoordinatedCarePlan_June2014.pdf
- 11. National Information Board of the UK. (2014). Personalised Health and Care 2020[Brochure]. Author. Retrieved from https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/384650/NIB_Report.pdf
- 12. The Most Innovative Patient Portal Features. (n.d.). Retrieved October 30, 2014, from http://www.healthworkscollective.com/charles-settles/317786/most-innovative-patient-portal-features
- 13. Topol, E. J. (n.d.). The patient will see you now: The future of medicine is in your hands.
- 14. Winslow, R. (2015, May 10). The WIreless Revolution Hits Medicine. The Wall Street Journal. Retrieved from http://www.wsj.com/articles/SB10001424052702303404704577311421888663472
- 15. Kish, L. J., & Topol, E. J. (2015). Unpatients—why patients should own their medical data. Nat Biotechnol Nature Biotechnology, 33(9), 921-924. Retrieved October 30, 2015.
- 16. Care Plan Project 2012. (2012). Retrieved from http://wiki.hl7.org/index.php?title=Care_Plan_Project_2012
- 17. The Expanding Role of Pharmacists in a Transformed Health Care System. (n.d.). Retrieved from http://www.nga.org/files/live/sites/NGA/files/pdf/2015/1501TheExpandingRoleOfPharmacists.pdf
- 18. Neal, L. (2007). Online health Communities. Proceedings of the Conference on Human Computer Interaction, 444-447.com/website/index.html
- 19. Phillips, L. (2015, April 21). What Will Health Care Look Like in 5-15 Years? Retrieved September 27, 2015, from http://www.hfma.org/Leadership/E-Bulletins/2015/April/What_Will_Health_Care_Look_Like_in_5-15_Years_/
- 20. Nurse Practitioners and Primary Care. (n.d.). Retrieved October 30, 2015, from http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=79
- 21. Heyworth, L., Rozenblum, R., Burgess, J. F., Baker, E., Meterko, M., Prescott, D., . . . Simon, S. R. (2014). Influence of Shared Medical Appointments on Patient Satisfaction: A Retrospective 3-Year Study. The Annals of Family Medicine, 12(4), 324-330.
- 22. M. O. (n.d.) Is a medical home in your future. Retrieved September 28, 2015, from http://health.usnews.com/health-news/patient-advice/articles/2015/03/09/is-a-medical-home-in-your-future
- 23. Where healthcare is now on march to value-based pay. (n.d.). Retrieved October 30, 2015, from http://www.modernhealthcare.com/article/20150128/NEWS/301289952
- 24. Benjamin, R. M. (n.d.). The National Prevention Strategy: Shifting the Nation's Health-Care System. Public Health Rep. Retrieved October 30, 2015, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3185312/
- 25. GoInvo. “Care Cards” (2016). Retrieved from www.carecards.me