National Cancer Navigation
The White House Calls for a Childhood Cancer Service
Earlier this year, the Biden-Harris administration announced a handful of new actions relating to the Cancer Moonshot goals to reduce cancer mortality rates and improve the lives of patients and survivors.
The first action listed is the creation of CC-DIRECT: Childhood Cancer: Data Integration for Research, Education, Care, and Clinical Trials — an initiative to support children, adolescents, and young adults throughout their cancer journey. Among other services, CC-DIRECT would provide patient navigation support to families, facilitate research participation, and establish a portable, shareable, standardized cancer health record.
The National Cancer Institute has been tasked with creating CC-DIRECT, and since April 2023, NCI has been laying the groundwork with their National Cancer Plan. Although their efforts and strategies are primarily focused on research, they have extended a call to action for contributions from across different sectors.
7 Underlying Problems in the US Cancer Space
Our research aims to organize cancer journey pain points and underlying problems to support decision-makers in evaluating the potential impact of solutions they devise. This work reflects what our team has learned so far and is not a comprehensive representation of all aspects of the cancer experience. Feedback and suggestions are welcome at CancerNavigator@goinvo.com.
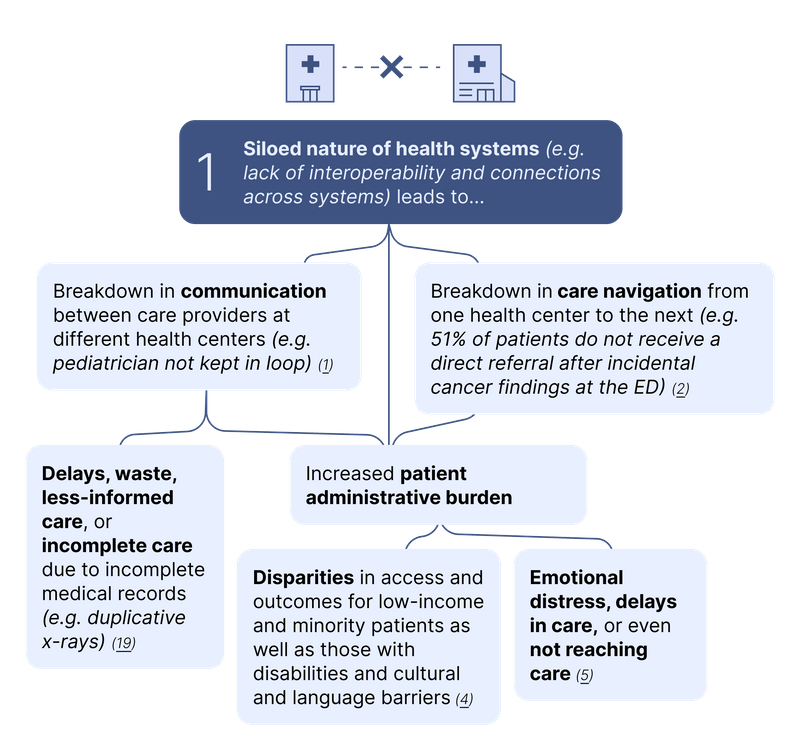
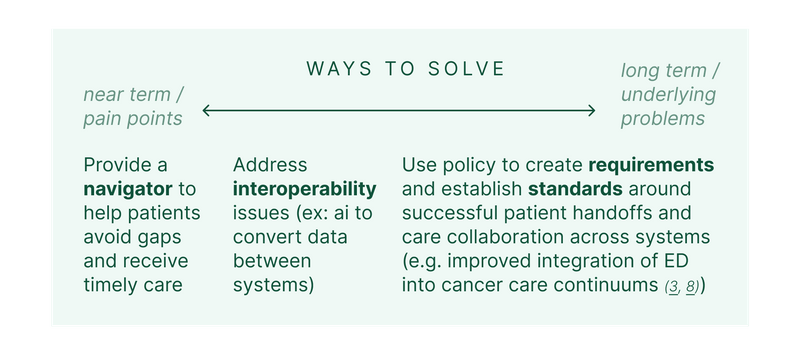
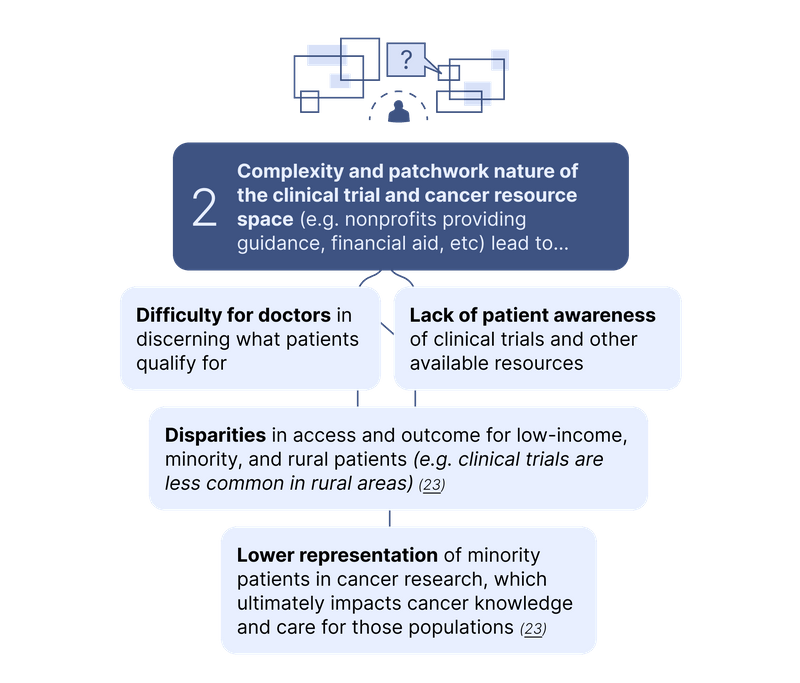
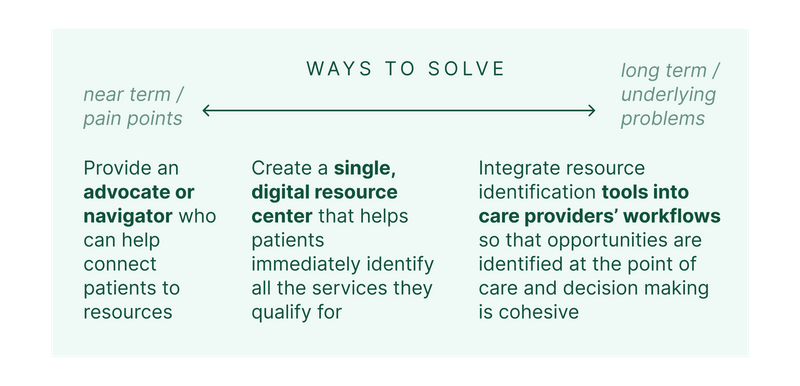
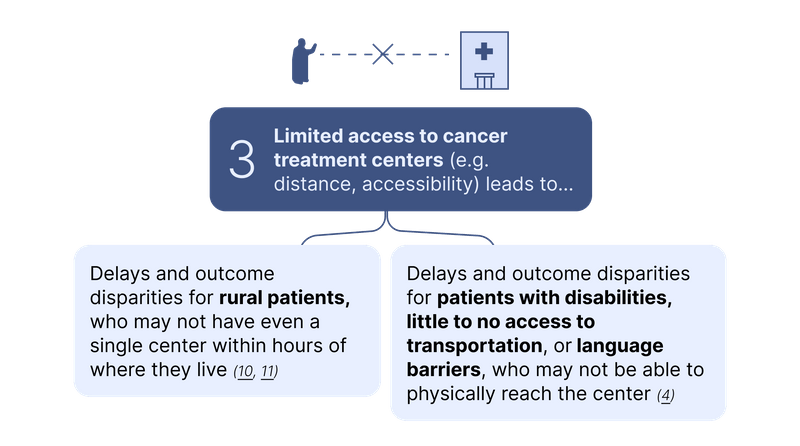
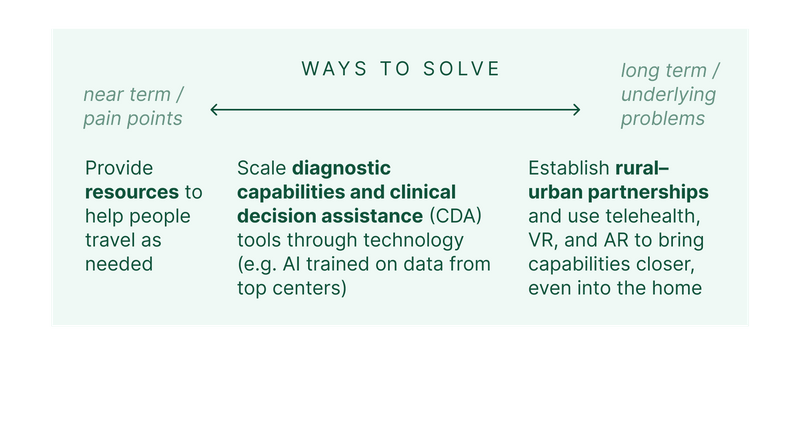
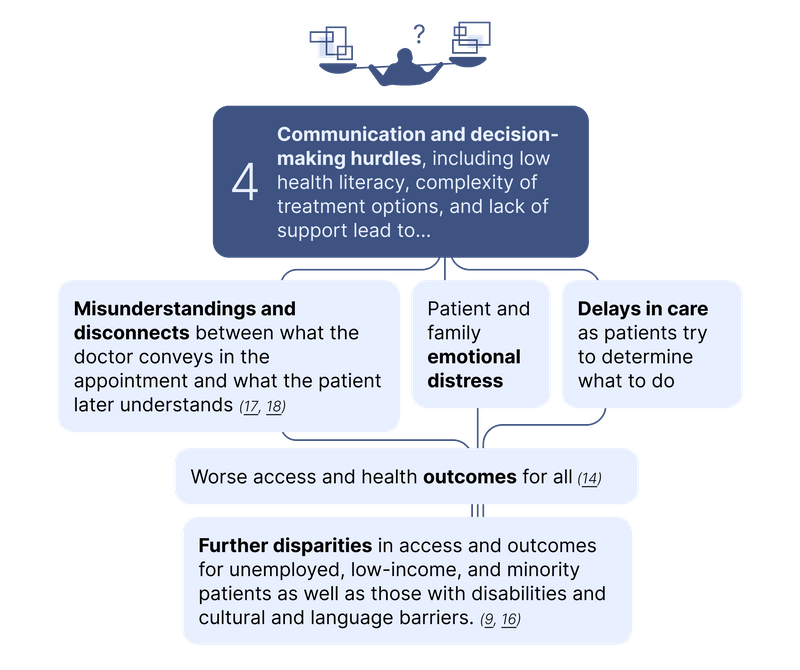
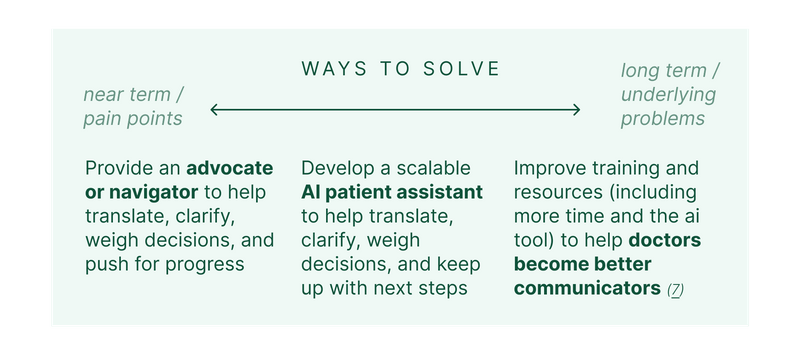
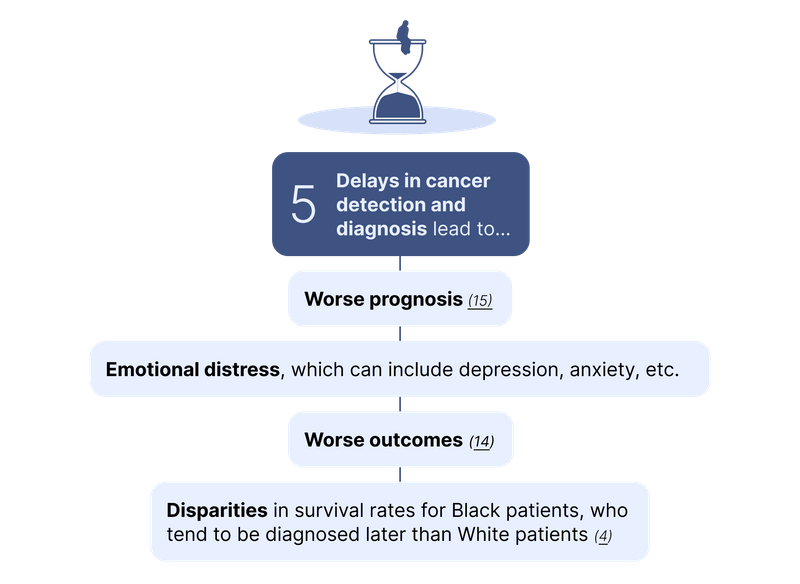
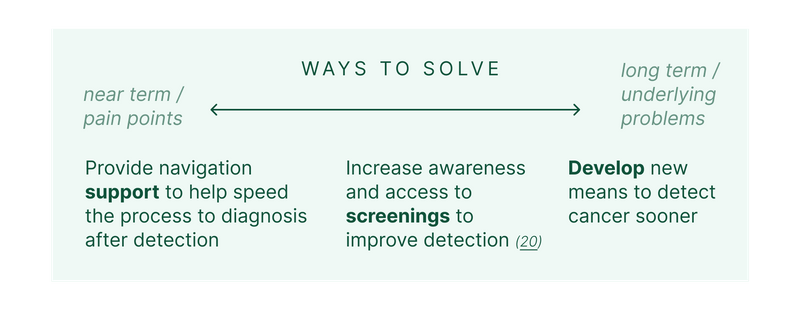
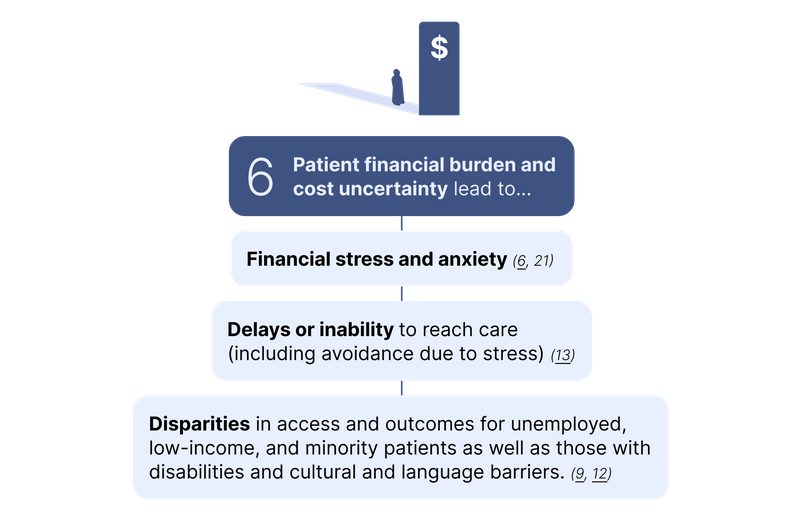
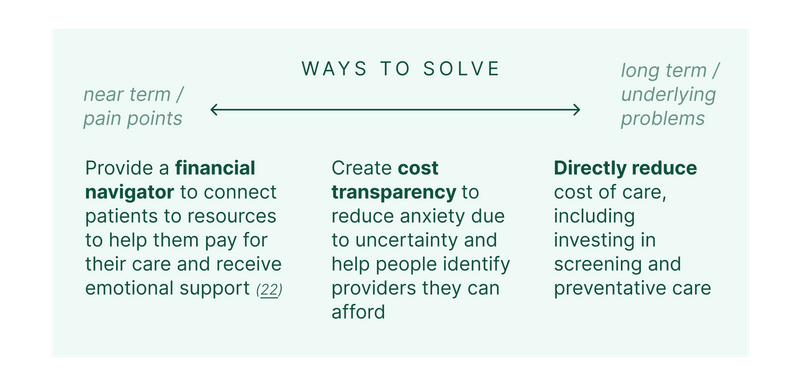
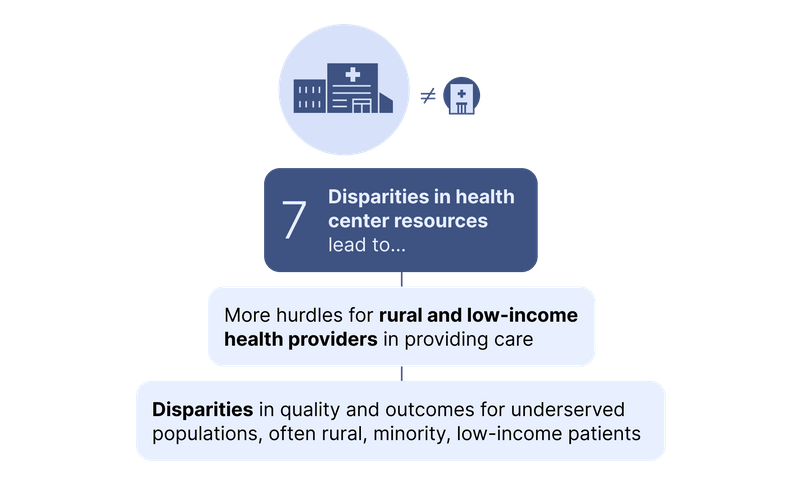
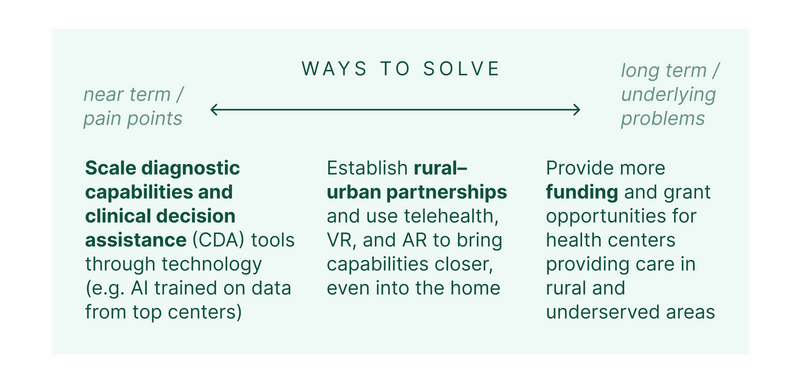
Disparities exist across all of these problem areas, disproportionately impacting individuals from low-income backgrounds, minority populations, and rural areas, as well as those with disabilities, language barriers, and cultural differences. Services must be designed around these communities' experiences from the outset if they are to be successful at closing the gaps. As we consider these problems, it’s helpful to identify the focus of a given approach: is it mostly intended to address the underlying, upstream problems, or the more immediate, downstream pain points?
The implementation of a national patient navigation service like CC-DIRECT could promptly address numerous pain points in cancer care, and research strongly highlights the significance and impact of human touch in patient care. In fact, the genesis of patient navigation resulted from a 1989 report by the American Cancer Society that found that poor cancer patients faced substantially greater barriers in obtaining care and often did not seek care they couldn’t afford. The following year, the Harlem Hospital Center implemented the first patient navigation program for underserved cancer patients, showing that patient navigation could dramatically improve outcomes.
By also expanding our attention to underlying problems like delays in detection and diagnosis and the siloed nature of health systems, we can decrease the volume of manual responsibilities for navigators and maximize the impact and scalability of patient navigation.
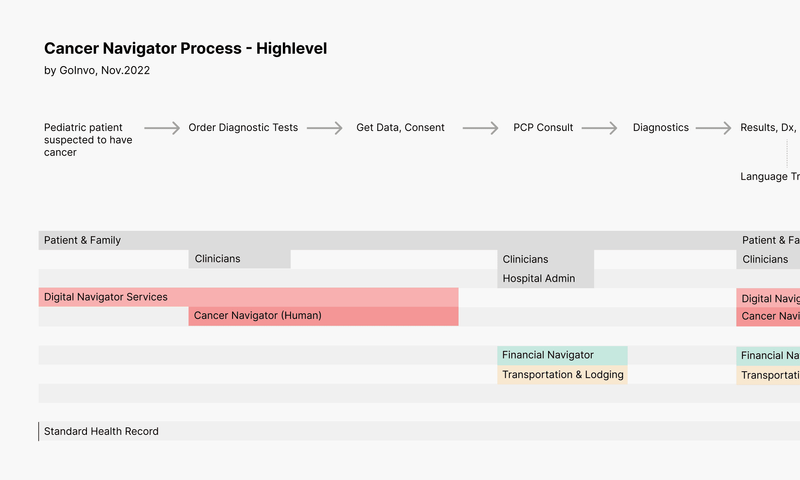
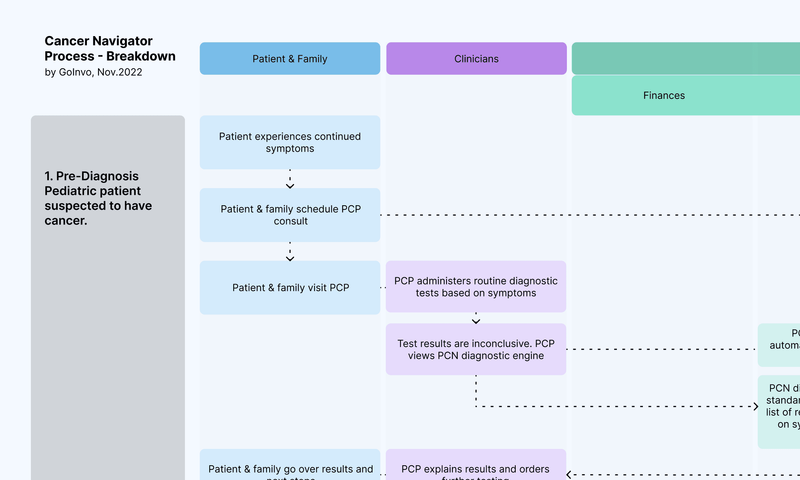
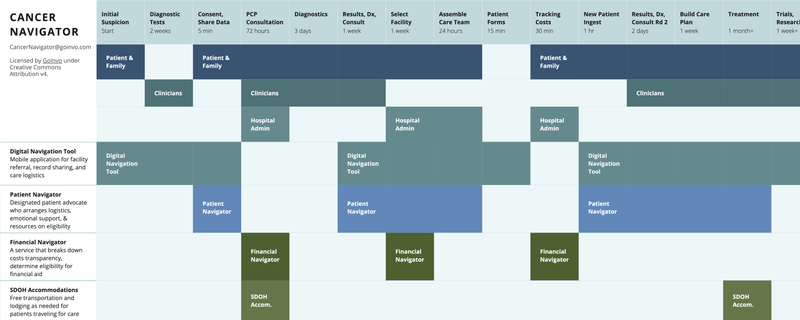
Reimagining Patient Navigation for Cancer
This timeline outlines how cancer navigation could look across multiple services, each of which is a direct response to existing issues with quality and experience of care for patients. These services include:
- Digital Navigation Tool
Mobile application for facility referral, record sharing, and care logistics - Patient Navigator
Designated patient advocate who arranges logistics, emotional support, and resources on eligibility - Financial Navigator
A service that breaks down costs transparency, determine eligibility for financial aid - SDOH Accommodations
Free transportation and lodging as needed for patients traveling for care - Patient Education
Resources to help patients further their understanding of their health - Standard Health Record
A longitudinal, shareable electronic health record
See our progress since November 2022
Have feedback? Send it to CancerNavigator@goinvo.com
Authors
Claire Lin
Tala Habbab
Sharon Lee
Craig McGinley
Samantha Wuu
Juhan Sonin
Contributors
Subscribe to our open source healthcare newsletter.
References
- Walsh, Jennifer, et al. “What Are the Current Barriers to Effective Cancer Care Coordination? A Qualitative Study.” BMC Health Services Research, vol. 10, no. 1, 20 May 2010: https://link.springer.com/article/10.1186/1472-6963-10-132
- Delamare Fauvel, Alix, et al. “Diagnosis of Cancer in the Emergency Department: A Scoping Review.” Cancer Medicine, vol. 12, no. 7, 9 Jan. 2023. Accessed 16 Apr. 2023: https://pubmed.ncbi.nlm.nih.gov/36622062/
- “Cancer and Emergency Medicine | EGRP/DCCPS/NCI/NIH.” Accessed 31 May 2023: https://epi.grants.cancer.gov/emergency-medicine/
- Tong, Michelle, and 2022. “Racial Disparities in Cancer Outcomes, Screening, and Treatment.” KFF, 3 Feb. 2022: www.kff.org/racial-equity-and-health-policy/issue-brief/racial-disparities-in-cancer-outcomes-screening-and-treatment/
- Zhu, J., et al. “First-Onset Mental Disorders after Cancer Diagnosis and Cancer-Specific Mortality: A Nationwide Cohort Study.” Annals of Oncology, vol. 28, no. 8, 19 May 2017, pp. 1964-1969: https://doi.org/10.1093/annonc/mdx265
- Carrera, Pricivel M., et al. “The Financial Burden and Distress of Patients with Cancer: Understanding and Stepping-up Action on the Financial Toxicity of Cancer Treatment.” CA: A Cancer Journal for Clinicians, vol. 68, no. 2, 16 Jan. 2018, pp. 153-165: https://doi.org/10.3322/caac.21443
- Fallowfield, Lesley, and Valerie Jenkins. “Communicating Sad, Bad, and Difficult News in Medicine.” Lancet (London, England), vol. 363, no. 9405, 2004, pp. 312-9: https://www.ncbi.nlm.nih.gov/pubmed/14751707
- Nazemi, Kellie J., and Suman Malempati. “Emergency Department Presentation of Childhood Cancer.” Emergency Medicine Clinics of North America, vol. 27, no. 3, 1 Aug. 2009, pp. 477-495. Accessed 31 May 2023: https://pubmed.ncbi.nlm.nih.gov/19646649/
- Hendren, Samantha, et al. “Patients' Barriers to Receipt of Cancer Care, and Factors Associated with Needing More Assistance from a Patient Navigator.” Journal of the National Medical Association, vol. 103, no. 8, July 2011, pp. 701-710: https://doi.org/10.1016/s0027-9684(15)30409-0
- “Rural Urban Disparities in Cancer.” Gis.cancer.gov: https://gis.cancer.gov/mapstory/rural-urban/index.html
- Onega, Tracy, et al. “Geographic Access to Cancer Care in the U.S.” Cancer, vol. 112, no. 4, 2008, pp. 909-918: https://doi.org/10.1002/cncr.23229
- Ward, E., et al. “Association of Insurance with Cancer Care Utilization and Outcomes.” CA: A Cancer Journal for Clinicians, vol. 58, no. 1, 1 Jan. 2008, pp. 9-31: https://doi.org/10.3322/ca.2007.0011
- Marlow, Nicole M., et al. The Relationship between Insurance Coverage and Cancer Care: A Literature Synthesis. PubMed, Research Triangle Park (NC), RTI Press, 2009: https://www.ncbi.nlm.nih.gov/books/NBK542737/
- Meijer, Anna, et al. “Effects of Screening for Psychological Distress on Patient Outcomes in Cancer: A Systematic Review.” Journal of Psychosomatic Research, vol. 75, no. 1, July 2013, pp. 1-17: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3833882/
- Kling, Jim. “Time to Cancer Diagnoses in U.S. Averages 5 Months.” www.mdedge.com, 15 Sept. 2022. Accessed 31 May 2023: https://www.mdedge.com/hematology-oncology/article/257891/breast-cancer/time-cancer-diagnoses-us-averages-5-months
- Handtke, Oriana, et al. “Culturally Competent Healthcare - a Scoping Review of Strategies Implemented in Healthcare Organizations and a Model of Culturally Competent Healthcare Provision.” PLOS ONE, vol. 14, no. 7, 30 July 2019, pp. 1-24: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0219971
- Nekhlyudov, Larissa, et al. “Patient-Centered, Evidence-Based, and Cost-Conscious Cancer Care across the Continuum: Translating the Institute of Medicine Report into Clinical Practice.” CA: A Cancer Journal for Clinicians, vol. 64, no. 6, 9 Sept. 2014, pp. 408-421: https://doi.org/10.3322/caac.21249
- Kessels, Roy P C. “Patients' Memory for Medical Information.” Journal of the Royal Society of Medicine, vol. 96, no. 5, May 2003, pp. 219-22: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC539473/
- Rosenkrantz, Andrew B., et al. “Perceptions of Radiologists and Emergency Medicine Providers Regarding the Quality, Value, and Challenges of Outside Image Sharing in the Emergency Department Setting.” AJR. American Journal of Roentgenology, vol. 214, no. 4, 1 Apr. 2020, pp. 843-852. Accessed 28 June 2021: https://pubmed.ncbi.nlm.nih.gov/32023121/
- Virnig, Beth A., et al. “A Matter of Race: Early-versus Late-Stage Cancer Diagnosis.” Health Affairs, vol. 28, no. 1, Jan. 2009, pp. 160-168: https://doi.org/10.1377/hlthaff.28.1.160
- “Survey: Majority of Cancer Patients Struggle to Afford Cancer Care.” American Cancer Society Cancer Action Network, 15 Dec. 2021: www.fightcancer.org/releases/survey-majority-cancer-patients-struggle-afford-cancer-care
- Robin Vanderpool, DrPH. “Availability and Accessibility of Cancer Care Delivery Approaches to Reduce Financial Toxicity of Rural and Urban Cancer Patients in Kentucky.” Www.jons-Online.com, vol. 13, no. 5, 1 June 2022. Accessed 31 May 2023: www.jons-online.com/issues/2022/may-2022-vol-13-no-5/4518-availability-and-accessibility-of-cancer-care-delivery-approaches-to-reduce-financial-toxicity-of-rural-and-urban-cancer-patients-in-kentucky
- Awidi, Muhammad, and Samer Al Hadidi. “Participation of Black Americans in Cancer Clinical Trials: Current Challenges and Proposed Solutions.” JCO Oncology Practice, vol. 17, no. 5, May 2021, pp. 265-271: https://doi.org/10.1200/op.21.00001